Residents of Joseph’s House, a home for homeless individuals with HIV and others with serious illnesses, gathered downstairs for a birthday celebration. Between bites of carrot cake and dancing to Stevie Wonder’s “Happy Birthday,” Robert Ramsey, a resident of the house, described how he came to terms with his diagnosis. An elderly African-American man who contracted HIV over 30 years ago, Ramsey seemed cheerful as he talked about his struggle with accepting his identity as others cast a judgmental eye.
“I didn’t want to face the fact that I had it,” Ramsey said. “I kept saying, ‘No, this ain’t true, this ain’t true. This ain’t true.’”
Even today, Ramsey said, many people get nervous when an HIV patient coughs near them.
“There’s a lot of embarrassment,” he continued. “You don’t want nobody to know that you got this thing. Because you’re afraid of being mistreated.”
Ramsey is one of thousands of Washington, D.C. residents who live with HIV. D.C.’s HIV rate is considered an epidemic. LaShawn, a middle-aged African-American woman who declined to give her last name, is an established member of the Joseph’s House community who has also experienced the shame firsthand. And while the stigma surrounding the disease has lessened in recent years, she said that more needs to be done to erase the ostracism of HIV patients.
“We deserve a chance just like anybody else; we don’t need to be looked at differently,” she said.
If it were a state, the District would claim the second-highest average income in the U.S. but would also have nearly the highest poverty rate, with almost 20 percent of residents under the federal poverty line. As housing prices continue to climb, the number of homeless residents has increased by nearly 28 percent since 2010. And despite having the second-highest rate of health insurance in the nation, D.C residents are nearly eight times more likely than the average U.S. resident to contract HIV in their lifetimes. Organizations like Joseph’s House, which assist HIV patients with their daily treatments, creating a sense of self, and finding a welcoming community, provide an important service in Washington.
LaShawn said that the strength of these organizations lies in their patient communities. Fellow HIV patients are often the first point of contact for those navigating a new condition and identity. LaShawn values assisting new residents because when she was diagnosed with HIV, others stepped in to to mentor her on living with the condition.
“With the residents here, if they’re feeling some type of way, if they might have a rash or something, they come to me and ask me questions, and I give them advice and tell them what medication they should ask their doctor for,” LaShawn said.
***
In 2007, the District had reached a dubious mark: 3 percent of residents were HIV positive. In 2009, Shannon Hader, the director of the D.C. HIV/AIDS Administration, told The Washington Post: “Our rates are higher than [those of] West Africa.”
From 1998 and 2007, Congress had blocked use of local tax dollars for needle-exchange programs, but after Congress lifted the ban, the return of the program had extraordinary results, said Jennifer Huang Bouey, an epidemiologist at Georgetown. Her research has focused on the determinants of health and health disparities among marginalized populations; she has also worked as a consultant for the Clinton HIV/AIDS Initiative.
“In 2007, 95 percent of the HIV positive in D.C. were associated with contaminated needles. So it’s mostly IDU [injection drug users],” Bouey said. “After D.C. government implemented a needle exchange, that really eliminated, or at least dramatically decreased, one of the highest risks.”
Now, even though the District’s infection rates have fallen a percentage point since their peak in 2007, many disparities still exist in terms of the populations affected by HIV. African-Americans continue to be disproportionately at-risk for contracting the virus, and individuals with intersectional minority identities are most at risk of contracting HIV.
“It’s a well-known fact that there are all sorts of barriers across racial groups [with regard to HIV prevention], but particularly among African-American men that prevent that from happening and there’s well known data out there that it’s really about social class and stigma and poverty,” said Michael Plankey, an epidemiologist at Georgetown University Medical School and a researcher at the Multicenter AIDS Cohort Study.
The data Plankey cited showed wide inequalities in the distribution of HIV among various groups. The two groups with the highest rates of infection D.C. are black men who have sex with other men (MSM), accounting for 27 percent of all HIV-infected residents, and black heterosexual women, at 16 percent, according to the Department of Health HIV/AIDS, Hepatitis, STD, and TB Administration’s 2017 report. Of new cases diagnosed between 2013 and 2017, those two groups combined make up 40 percent of HIV-positive residents, and 4.4 percent of African-American men in D.C. live with the disease. White MSM make up 14 percent of District residents living with HIV and 12 percent of the new HIV cases reported over those four years.
***
Human immunodeficiency virus is transmitted through body fluids during sexual intercourse, contact with blood, or from mother to child during pregnancy or childbirth. Over time, if the infected individual does not receive treatment, HIV will progress into acquired immunodeficiency syndrome or AIDS.
Without treatment, an HIV-infected individual has an average life expectancy of 11 years from the time of infection; an untreated AIDS diagnosis has a prognosis of several months to two years. There is no cure or HIV vaccine, but a person with the condition can live a near-normal lifespan if they start antiretroviral treatment in the early stages and continue for the rest of their life.
“Now we’ve got evidence that if you take your medications and you’re virally suppressed, the likelihood that you’re going to transmit to anybody is nearly zero,” Plankey said. “This whole thing of U equals U, undetectable is un-transmissible, is really where we’re going,”
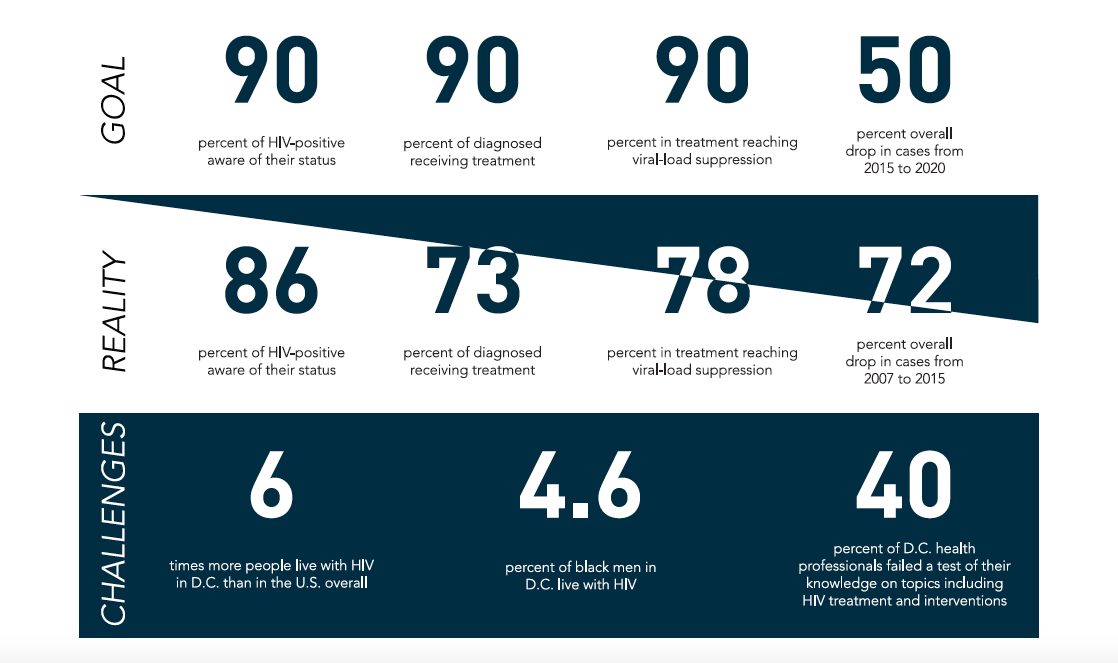
‘U equals U’ has been a central tenet of the D.C. government’s approach to fighting HIV/AIDS, highlighted by Mayor Muriel Bowser’s administration’s ‘90-90-90-50’ plan, announced in 2015 and orchestrated in conjunction with DC Appleseed and the Washington AIDS Partnership. The goals of the scheme are that, by 2020, 90 percent of HIV-positive District residents know their status, 90 percent of residents living with HIV are in treatment, 90 percent of residents with HIV in treatment reach viral load suppression, and there is a 50 percent overall reduction in new HIV cases from 2015’s mark of 401.
Importantly, improving access to treatment is just a component of the fight against HIV/AIDS; the other component is prevention of HIV. Pre-exposure prophylaxis, or PrEP, is the use of drugs to protect individuals who may participate in “high-risk” behavior. PrEP has been shown to be clinically effective in reducing rates. According to the CDC, PrEP reduces the chance of HIV infection by up to 92 percent. But PrEP has unequal distributional outcomes, as black men are less likely to get this service, Plankey said. Several studies support his claim, including a 2018 report by the CDC that found “while two-thirds of people who could potentially benefit from PrEP are African-American or Latino, they account for the smallest percentage of prescriptions to date.” LaShawn believes that a lack of education, spurred by inadequate advertising, drives low uses of PrEP among high-risk communities, but also that the problem goes beyond education. Once again, stigma plays a role, though many try to overcome it.
“They don’t know about it, that’s true, and then when they do know about it, and they want it, it’s kind of hard for them to get it,” LaShawn said. “Even if people might not want to say ‘yo I’m going to go get that’ on the low-low people will go get it. You know, you’d never know if they’re taking it or not.”
Nationwide, these trends in the District fit into a larger picture of racial disparities in HIV cases. A recent CDC report, based on data from 2014-15, found that African-Americans accounted for 39 percent of new cases in the Northeast, 50 percent in the Midwest, and 54 percent in the South. The western United States was the only region where African-Americans were not the group most at-risk for contracting HIV (Latinx people were, at 39 percent).
Bouey’s research into HIV has centered on the second most at-risk group, black heterosexual women. A systematic problem with HIV intervention in D.C. and the United States, says Bouey, is the refusal to recognize the presence of sex work and its connection to HIV. In fact, the United States is one of the only countries that doesn’t have proper HIV surveillance of female sex workers, she said. Though heterosexual women are ordinarily not high-risk for HIV, the lack of surveillance in the U.S. and the District has led African-American heterosexual women to be more vulnerable.
“In D.C., part of the problem is people don’t want to face the issue that many of these low-income, black women are in and out of the commerical sex transaction,” Bouey said, referring specifically to the women in her HIV prevention study which focuses on commercial sex workers.
LaShawn interjected when asked whether she knew any sex workers with HIV.
“Me, me,” she said, and later added, “I was homeless so I was doing it to eat, to put clothes on my back, you know.”
Bouey worked with D.C. Helping Individual Prostitutes Survive (HIPS), a harm-reduction organization, to conduct a study of 32 black heterosexual women, both cisgender and transgender, who had been street-based sex workers. Specifically, Bouey was interested in finding out about PrEP and HIV testing among these women. With regard to the latter, they found that most women knew their status, which was HIV-positive for about 30 percent of the respondents.
“Quite consistent with the report from D.C., we found that they have very good HIV testing records,” Bouey said. “Almost 90 percent have been tested for HIV, and we’ve found that they have a very high HIV prevalence, over 30 percent.”
The findings also revealed that few of the HIV-positive women were undergoing any treatment. Hardly any of the women knew about PrEP, which would have served a logical purpose given their profession, said Bouey.
“We asked them about whether they have treatment, and less than half are enrolled in treatment,” Bouey said. “That’s a problem.”
“We found that not many of them have heard of PrEP, even though DC has done a mass media campaign to promote PrEP among women,” she continued. “Some of them are like ‘I have heard of it, or seen the signs for it on the bus, but I don’t know what it is. Is it a job training program?’”
What remains unclear are the root causes of under-treatment and lack of knowledge about PrEP, consistent with both Dr. Plankey’s and Dr. Bouey’s findings. It’s not insurance, as the District has a high rate of coverage and these women’s insurance would cover the treatment, nor is it eligibility for these programs. A little over 10 percent of the survey’s respondents believed they were eligible for PrEP, said Bouey, but in fact, all of them were covered for it. Bouey inferred from her findings that primary-care physicians don’t do an adequate job of referring their patients to the correct outlets.
“The problem is, these primary care physicians don’t know these women are high-risk,” Bouey said. “They don’t talk about their lifestyle on the street.”
“There’s a fear from both sides,” Bouey continued. “The women have really internalized the stigma – first of all it’s illegal, and then they feel a lot of shame. From the physician side, they don’t know what to ask.”
***
On one hand, Washington’s falling HIV rates constitute an undeniable success story, the result of an effective public health campaign and heightened awareness. Yet the District is not on track to accomplish its prescribed goals by 2020; in particular, reducing the number of new cases. The goal of a 50 percent reduction seems a long way off, as the number of new cases has stayed around 370 per year, close to 2015’s mark of 400.
The challenge now for policymakers and advocates is to address the undeniable imbalance in not only HIV infection rates, but access to vital pre- and post-diagnosis treatment. Combating HIV’s stigma is connected to the solution, says Bouey, citing the women she encountered in her research.
“When you talk to these women, they’re not monsters, lazy women,” Bouey said. “We’ll continue to battle the stigma these women face every day, and try to humanize these women, to let more people understand the challenges they face.”
LaShawn recalled her others’ reactions when she first learned her diagnosis, almost 30 years ago. She said that she got the virus from her ex-husband.
“People didn’t even want to touch you,” LaShawn said. “They thought they was going to get it, they weren’t educated, they didn’t know.”
Ramsey offered advice for both people unfamiliar with HIV patients and those living with the disease.
“[What] I want them to know is that when a person have HIV, he is not a threat to you,” he said. “And that people that have HIV must definitely know there is life after HIV,” Ramsey continued.
LaShawn said that she no longer hides her diagnosis; it is a part of who she is.
“I’m not ashamed that I have it,” she said. “It’s like a stray bullet, it has nobody’s name on it.”